190
Views & Citations10
Likes & Shares
MATERIALS AND METHODS
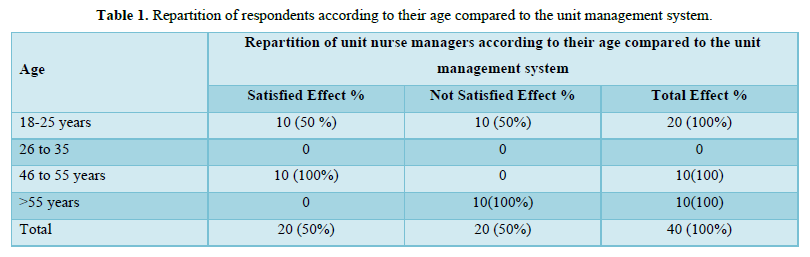
This descriptive study conducted with nurses working in Aru and Bunia hospital, Ituri Province from September 2022-to Mars 2023. The sample comprised 100 (out of 120) nurses working in the public hospitals for a minimum period of three months and 80 nurses randomly selected accepted to participate in the study. The participation rate was 66,6%. Data collection was through a questionnaire. The form consisted of two parts: the first collected information on the descriptive and occupational characteristics of nurses, and the second data on the nurse's knowledge levels in the management of unit care. Ten (10) questions formed to measure the knowledge levels and satisfaction of nurses submitted, response was evaluated as 1 point for true and false and 0 points for unknown. The total points are calculated by adding points taken from all the answers. Regarding the number of points for knowledge questions, the minimum was 0 and 10. The nurses who correctly replied to less than half of the questions classified as having an insufficient knowledge level, those who correctly answered 50-75% of the questions classified as having an intermediate knowledge level, and those who correctly replied to 75-100% of the questions classified as having a sufficient knowledge level. Accordingly, the nurses scoring ≥19 points were certified as having a good knowledge level, those scoring between 13 and 18 points were certified as having an intermediate knowledge level, and those scoring ≤12 points were certified as having an insufficient knowledge level. Before joining, the forms were distributed to the nurses only after they provided information about the study and by taking their verbal consent. The questionnaire forms, which took 15-20 minutes to fill, were given to the nurses by the researchers, and the nurses were requested to fill in at an appropriate time.Repartition of unit nurse managers according to the age compared to the unit management system (information/communication regarding illness, medication, services organization, appreciation of quality care, condition or length of hospital stay of patients, socio-demographic characteristics of the patients, and of their behavior, the dimensions of nursing care such as information given by nurse, interpersonal relationship, technical quality of nurse, and physical environment.In Table 1, the findings show that 100% of better management of unit care was observed amongst nurses aged between 46 and 55 years and were satisfied with the management system followed by 50% of those whose ages vary from 18 to 25years.
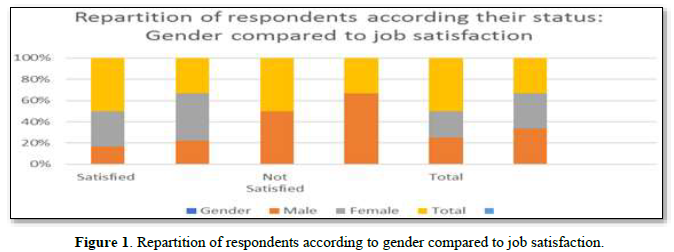
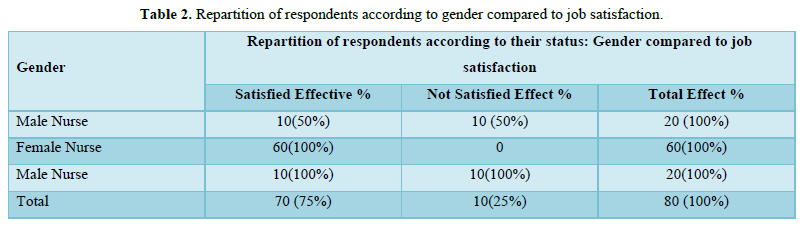
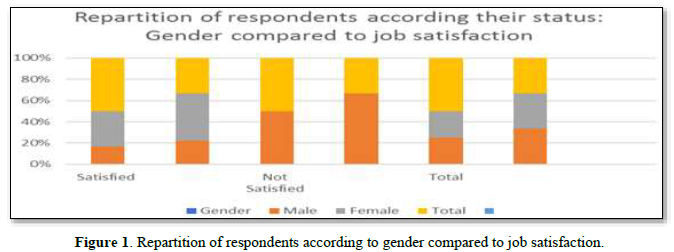
In Table 2, the findings related to gender compared to job satisfaction in managing unit care show 100 % of the female nurse were satisfied with the health management systems in units under their responsibilities. In the same table, 50% of the male nurses satisfied while others not (Figure 1).
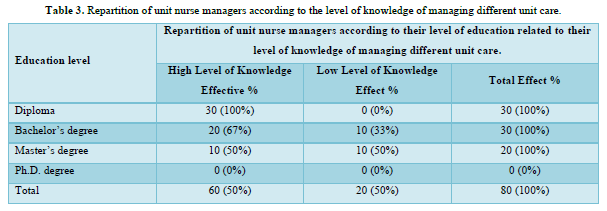
In Table 3, the findings revealed 100% of nurses with a diploma showed a high level of knowledge in managing unit care, and 100% with a bachelor’s present have poor followed by 50% of those with master’s degree.
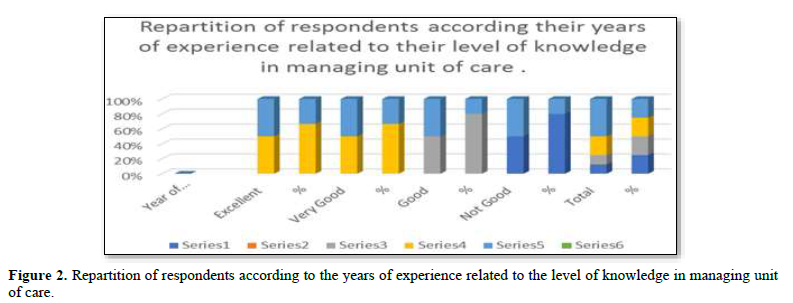
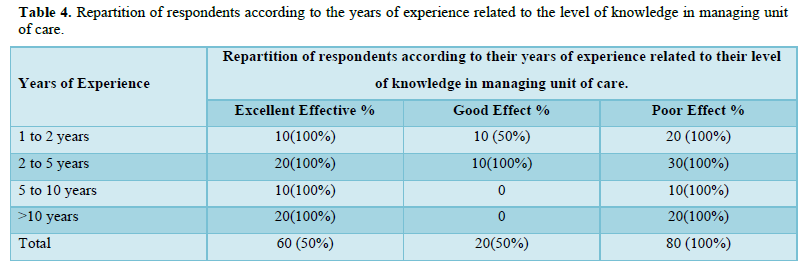
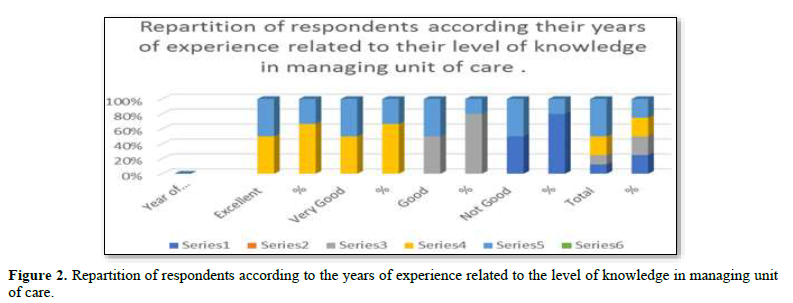
Regarding the years of experience, in Table 4 & Figure 2, the findings show that 100 % of bad practices in managing unit care observed amongst nurses with less than two years of experience, experience but 100% of nurses exceeding two and ten years presented good knowledge in managing the unit under their responsibilities.
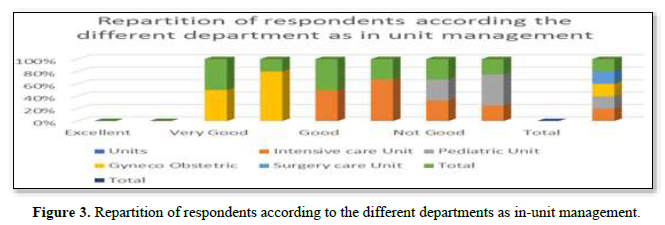
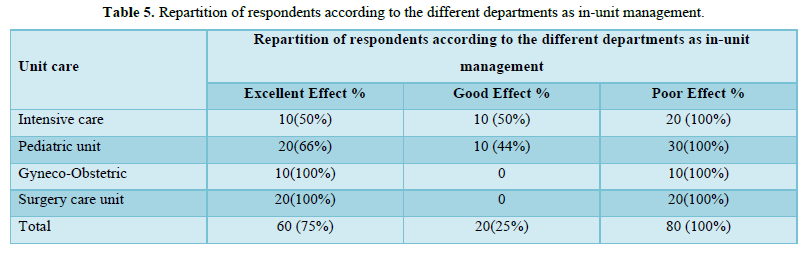
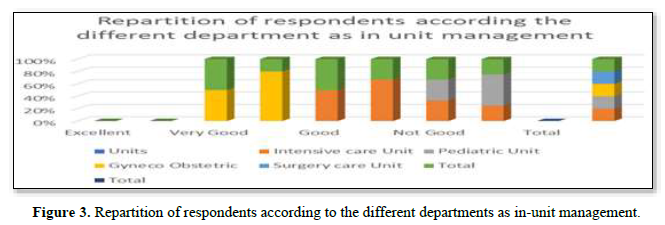
In Table 5, the findings show that 100% good management of unit care observed amongst nurses in Gyneco- Obstetric department, but nurses managing pediatric unit exceed quotations 100% not good, half of the nurses (50%) in Intensive care presented good management and another half (50%) present poor management in the same unit (Figure 3).
DISCUSSIONS
The results of this project show in Table 1, 100% of satisfied management of unit care observed amongst nurses aged forty-six followed by 50% of age between 18 to 25years. Good unit management observed amongst nurses’ conscious of their responsibilities assigned they considered the work part of their life, do with devoutness, sweetheart, etc. We can corroborate this argument by the results of Boyle [8] in which they determined that the way the leader coordinates nursing work had a direct link to nurses’ satisfaction and nurse leaders’ position of power within the unit, and leader’s influence in the daily coordination of nursing work within the unit management [8]. In Table 2, important finding of the study is staff nurses’ perceptions of managers associated with their perceptions of the organization. The participative management style demonstrated similar positive results found in earlier work on leadership and retention completed by Volk & Lucas [9]. These three studies recommended nurse managers be involved in leadership training and specified that nurse managers need to learn how to develop a participative management style [10]. The junior nurses associated in the tandem with senior nurses as participative management to let junior gain experience and avoid the dissatisfaction of patients [11]. Connelly conducted individual studies investigating affiliation and recognition in leaders. Results from both studies were similar, demonstrating that affiliation, appreciation, and recognition by key leaders’ components of nurse retention. The findings revealed a primary reason for nurses remaining in a job was group cohesion, a sense of belonging, and an ability to relate openly with their managers [12]. According to the study examined the relationship between nurse managers’ personalities and staff nurses’ perception of their leadership style, power, and influence. Findings showed a correlation between nurse manager personality traits of extroversion motivation to manage. In Table 2, important finding of the study is staff nurses’ perceptions of managers associated with their perceptions of the organization. Participative management style demonstrated similar positive results found in earlier work on leadership and retention completed by Volk & Lucas [9]. Three studies recommend nurse managers be involved in leadership training and specified that nurse managers need to learn how to develop a participative management style [11]. In Table 2, results related to gender show 100 % of female nurses were satisfied with the health management system under their responsibilities in Bunia and Aru Hospital (50%) of male nurse were satisfy. Health planning proposed way expected to follow to attain well-being. It involves women and men setting goals, developing strategies, and managing units. New policy in public management reform in the DRC, the health system, is moving to the direction of financial decentralization, making the provinces directly responsible for health services. The leadership management should not be the empennage of women or men work hand to hand in planning, implementing, monitoring, and evaluating the primary health care strategy in accordance with the National Health Policy.
And in Table 3, the findings revealed that 100% of nurses with a diploma showed a high level of knowledge in managing unit care, followed by 67% of those with a Bachelor and 50% of master’s degree. In the same the level of education, 33 % with a bachelor’s present poor knowledge.
Nurse with secondary level interested in apprehending new skills in the nursing system from elders as novice may be one of their motivations. Besides, Nurses high education consider themselves educated know everything while not [12-14]. The fact can explain the findings of the eight researchers Force [14]. Dunham [12] identified five themes with implications for nursing leaders who wanted to promote job satisfaction and retention and transformational leadership styles. Dunham [12] and Force [14] positive extroverted personality traits magnet hospitals’ organizational structures. Goddard [15] having tenure in the organization, combined with advanced graduate education and managers who encouraged an atmosphere of autonomy, shared governance, group cohesion, and empowerment of staff with reward and recognition. Dunham-Taylor [16] said nursing staff who perceived their managers to exhibit transformational behaviors demonstrated a sense of empowerment. According to the research, the high job satisfaction associate with staff higher transformational leadership scores in executive nurses. Professional education (master’s, doctoral degree in nursing suggests strengthening an individual’s transformational characteristics [12]. In the second part of their study, a structured interview with 81 nurse executives asked two open ended questions about excellence in nursing leadership and the leader’s individual strengths and weaknesses. Finding differentiated the relationship between transformational leadership and transactional leadership. In the study, results suggest leaders have leadership characteristics from both transformational and transactional leadership styles [12]. Goddard [15] Medley & Larochelle [16] also investigated the relationship between the head nurse’s leadership style and staff nurse job satisfaction using a correlation study design. The Author pointed out nurse managers who want to exercise nursing leadership with the leaders needs in daily work acknowledge staff’s professional competency and promote professional growth [16]. In Table 4, in the findings, it’s found 100 % of bad practices in managing unit care observed amongst nurses with less than2 year of experience, and 100% of nurses with years of experience from 2 and 10 years presented good knowledge in managing the unit under their responsibilities. A study by Merve [17] in Department of Chest Diseases, İstanbul Bilim University School of Medicine, İstanbul, on Nurses’ Knowledge Levels of Chest Drain Management, in an Intensive care Unit. In this study, 69.3%, 37.9%, 26.1%, and 2.6% of the nurses stated that they obtained information on the management of patients with chest tubes from their colleagues, from the Internet, from books/ journals, and school education, respectively mean age was 32.08 years (SD: 8.24), vary between 22 and 53 years 35.3% nurses had an occupational experience between 1 and 5 years half had the same institutional experiences (49.7%). The scores of the nurses working in operating rooms were higher than those working in general services with an occupational experience of 16-20 years scored high records. Nurses in Bunia and Aru Hospital with less than 2years of experience could adhere to this theory to perform their knowledge by searching information from their colleagues, the Internet, and books, as done by their colleagues in Istanbul. In Table 5, the findings show 100% good management of unit care observed amongst nurses in Gyneco- Obstetric department, nurses managing pediatric unit exceed with quotations 100% not good, half (50%) in Intensive care presented good management and another half (50%) present poor management in the same unit to compare findings done in Istanbul where utmost of nurses was female (80%, n=124) 34.6% of nurses stated that they encountered at least one patient with a chest tube every day, and 32.7%, 32%, and 35.3% perceived their knowledge level about the management of patients with chest tubes as sufficient, intermediate, and insufficient, respectively 69.3%, 37.9%, 26.1%, and 2.6% of nurses obtained information about the management of patients with chest tubes from their colleagues, from the Internet, from books/ journals, and school education, respectively. The scores obtained by the female nurses were higher than those obtained by the male nurses; the difference between these scores was not statistically significant (p>0.05) with an associate degree scored high than those having a bachelor's degree, and the nurses working in surgical units scored higher than those working in internal medicine units; the difference between these scores was statistically significant [17].
CONCLUSION
The objective the paper is to examine how nurses manage units under their responsibilities in Bunia and Aru Referral Hospital to support local health authorities in deciding on nursing leadership and management in different health centers in Ituri Province. One month based on qualitative and quantitative data collection in Bunia and Aru Hospital assigned in managing units were interviewed and observed. Respondents randomly selected from 12 different units, collected data were gathered through interviews and observations conducted in four out of twelve randomly selected units, each consisting of seven participants analyzed by Excel using numbers and percentages. The findings show100% management of unit care is amongst nurses aged between 46 and 55 years, 50% satisfaction in the management system between nurses of 18 to 25 years and 100% of nurses 2 to 10 years old are perceived and have good impressions. Further, results (100 %) of bad practices in managing units observed amongst nurses with less than two years of experience, the demand for health services and nurses continuously growing, ageing populations and burden of chronic diseases, such as diabetics, hypertension, cancer, etc. and the health technology is ever-expanding, conclude as so far, regular debriefing of nurses on trimester or semester basis on knowledge and management in nursing to empowering staffs with new communication and technology skills, medication, services organization, appreciation of quality care, condition or length of hospital stay of patients, interpersonal relationship, technical quality of nurse, and physical environment of the hospital should be as of priority for Bunia and Aru Hospital. Many studies prove leadership is complex phenomenon, acknowledged by the multiple variables. In Cook's research, when reviewing leadership articles proposes solutions. He identified the focus for future development in nursing needs to be upon the change from a traditional hierarchical structure to one promoting an entrepreneurial spirit through transformational leadership.A move from the traditional and somewhat rigid hierarchical leadership model that he considered was operating within nursing at a time, aligned with transactional leadership [18]. Leadership, like job satisfaction, is a complex phenomenon studied quantitatively and qualitatively.- McCarthy G, Fitzpatrick JJ (2009) Development of a competency framework for nurse managers in Ireland. J Contin Educ Nurs 40(8): 346-350.
- McCarthy G, Fitzpatrick JJ (2014) Summary and future directions. In Fitzpatrick J.J., McCarthy G. (eds.), Theories Guiding Nursing Research and Practice. pp: 355-361.
- National Preventative Health Task Force (2009a) Australia the healthiest country by 2020. Technical Report 1 Obesity in Australia: A need for urgent action. Including addendum for October 2008 to June 2009. Available online at: www.health.gov.au/internet/preventativehealth/publishing.nsf/Content/tech-obesity
- Aiken LH, Sermeus W, Van den Heede K, Sloane DM, Busse R, et al. (2012) Patient safety, satisfaction, and quality of hospital care: Cross-sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ 344: e1717.
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber J (2002) Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA 288: 1987-1993.
- Scoble KB, Russell G (2003) Vision 2020, Part1. J Nurs Adm 33(6): 324-330.
- Wilson C (2005) Improving Teaching through Lesson Study. Teach Educ Q 32: 77-92.
- Boyle DK, Bott MJ, Hansen HE, Woods CQ, Taunton RL (1999) Managers' leadership and critical care nurses' intent to stay. Am J Crit Care 8(6): 361-371
- Volk MC, Lucas MD (1996) Relationship of management style and anticipated turnover. Dimens Crit Care Nurs 10(1): 35-40.
- Connolly P (2007) Qualitative Data Analysis in Education: A critical introduction using SPSS. London: Routledge.
- Hansen HE, Woods CQ, Boyle DK, Bott MJ, Taunton RL (1995) Nurse manager personal traits and leadership characteristics. Nurs Adm Q 19(4): 23-35.
- Dunham-Taylor J (2000) Nurse executive transformational leadership found in participative organizations. J Nurs Adm 30(5): 241-250.
- Dunham-Taylor J, Klafehn K (1995) Identifying the best in nurse executive leadership. Part1, Questionnaire results. J Nurs Adm 25(6): 68-70.
- Force MV (2005) The relationship between effective nurse managers and nursing retention. J Nurs Adm 35(7/8): 336-341.
- Goddard MB, Laschinger HK (1997) Nurse managers’ perceptions of power and opportunity. Can J Nurs Adm 10(2): 40-66.
- Medley F, Larochelle DR (1995) Transformational leadership and job satisfaction. Nurs Manag 26: 64-65.
- Merve T, Songül A, Gökduman, Abdülkadir A, Levent D (2016) Nurses’ Knowledge Levels of Chest Drain Management: A Descriptive Study. Eurasian J Pulmonol 18: 153-159.
- Cook MJ (1999) Improving care requires leadership in nursing. Nurse Educ Today 19: 306-312.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Allergy Research (ISSN:2642-326X)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- Journal of Rheumatology Research (ISSN:2641-6999)